Identifying critical clinical needs and evaluating the ability for existing technologies, as well as methodologies, to address these needs is of utmost value to healthcare innovation. The actual evaluation results determine whether solutions are adequate, need further adaptation, or are non-existent and require new scenario planning and development. These last two categories provide opportunities for innovation in both technology, methodology and/or concepts.
Looking at maternal and infant health, the HIMSS Innovation Committee discovered how innovation partnerships and new use case approaches can help drive actionable insights about infant mortality risk factors, provide opportunities to address disparities in preterm birth rates and narrow inequity gaps in health outcomes.
HIMSS defines healthcare innovation as the introduction and/or implementation of a usable concept, idea, service, process or product that improves at least one of the following: treatment, diagnosis, education, outreach, prevention or research. Innovation is frequently framed with a focus on invention of new technical products, processes or services. While the “build it and they shall come'' approach has driven scientific research and technological advancements, significant challenges remain. The opportunity for unlocking new opportunities for value creation seems to require shifting the focus from development and dissemination of new technologies to working across the healthcare ecosystem, i.e., patients, physicians, payers, providers, communities, etc., to identify and address both the unmet clinical needs and the unstated, unmet health needs.
In shifting the approach from how we make new technology fit into our healthcare system to address problems we need to solve. The HIMSS Innovation Committee explored many facets open for innovation including clinical care, finance, research, social determinants of health (SDOH) and patient/provider experience. Many problems we need to solve were identified, some unique to local healthcare providers and others that are more universally experienced. Rather than working with generalities and hypotheticals, we approached the challenge of global preterm birth by focusing on real-world case studies that illustrate how to define the problems, how to identify innovative solutions, and how to identify solutions that already exist and innovations that need to be developed.
The Innovation Committee selected the Quadruple Aim to classify needs-based problems because of its widespread adoption as an aspirational model for improving healthcare. In the initial phase this work, the committee recognized that research was not explicitly referenced in the Quadruple Aim. To address this, we adopted a framework that included the Quadruple Aim plus research.
The Innovation Committee sought feedback and validation of the framework as well as input regarding the case studies from key HIMSS committees including the Physician Committee, Nursing Informatics Committee, and Public Policy Committee, and the chair of the Social Determinants of Health Task Force. Additional global perspectives were provided by external subject matter experts.
Based on this broad-based input the Innovation Committee reworked the list to better balance clinical care, finance, research, patient/provider experience, and the SDOH. Additionally, reference to care providers was made more inclusive to reflect the importance of patient-focused clinical teams by referencing “the care team,” rather than any individual clinician roles. The criteria for case studies included: a well-defined clinical issue characterized by complex clinical, financial and social issues for which innovative thought, process and technology would improve outcomes.
This analysis has laid the groundwork for examining, in depth and in consultation with clinicians and researchers, two real-world use cases that present complementary but different approaches to the challenges associated with preterm birth, for the mother and child. Use Case 1 calls for consideration of the broad range of critical factors, including cultural and environmental, to better identify complexities and challenges upfront for successful implementation of innovative technologies. Use Case 2 provides an example of specific innovative technology developed through a well-defined understanding of the current state. Note that in both use cases, the focus is on the journey of the patient and interactions with the healthcare ecosystem and the opportunities for innovation to impact outcomes and improve those journeys.
Defining the Problem of Preterm Birth, a Global Challenge
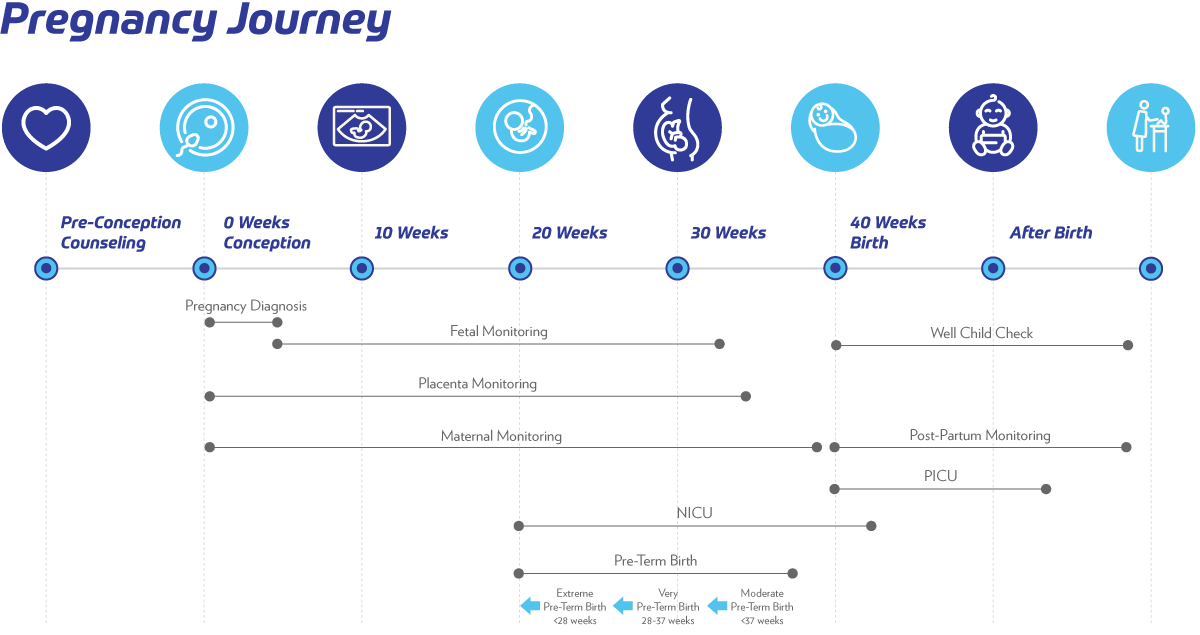
According to the World Health Organization (WHO), preterm birth is a live birth that occurs before 37 completed weeks of pregnancy. Preterm birth is further classified as extremely preterm (<28 weeks), very preterm (28 to <32 weeks), and moderate (32 to <34 weeks) to late preterm (34 to <37 weeks). Preterm birth may occur spontaneously or be initiated by a provider through induction of labor or elective caesarean delivery which may or may not be medically indicated.
A baby born after 37 weeks of pregnancy is not considered preterm; however, it is recommended that unless medically indicated, a pregnancy should be allowed to continue until 39 completed weeks to ensure optimal health outcomes of the baby. A significant healthcare problem, in the U.S. and globally—particularly critical in developing countries—is the issue of prematurity and stillbirths.
In many developing countries mother and infant mortality are the number one cause of premature death, thus impacting public health, safety, economic development and healthcare costs. In the U.S., approximately 11% (450,000) of all births are premature and this numbers 15,000,000 globally. Additionally, stillbirths occur in approximately 0.3% (24,000) pregnancies in the U.S.
There are variations in preterm birth rates by geographic region, socioeconomic status, demographics, and education that may impact health outcomes and costs. When countries are grouped by their World Bank income categories, it is found that approximately 90% of all preterm births occur in low‐ and middle‐income countries.
Adverse infant health outcomes and disparities call for action. Stillbirth is not only a challenge for poor countries. In 2019, 39 high-income countries had a higher number of stillbirths than neonatal deaths. A mother’s level of education and access to timely high-quality healthcare tends to be the greatest drivers of inequity in high-income countries.
In both low- and high-income settings, stillbirth rates are higher in rural areas than in urban areas and disparities exist among racial and ethnic groups. For example, Inuit populations in Canada have been observed to have stillbirth rates nearly three times higher than the rest of Canada. Infant mortality rates are high for African American Blacks, American Indians, and Native Alaskan populations. African American women in U.S. have nearly twice the risk of stillbirth compared to White, Asian, Hispanic or Pacific Islander mothers. In Nepal, women of minority castes had stillbirth rates 40-60% higher than women from upper-class castes.
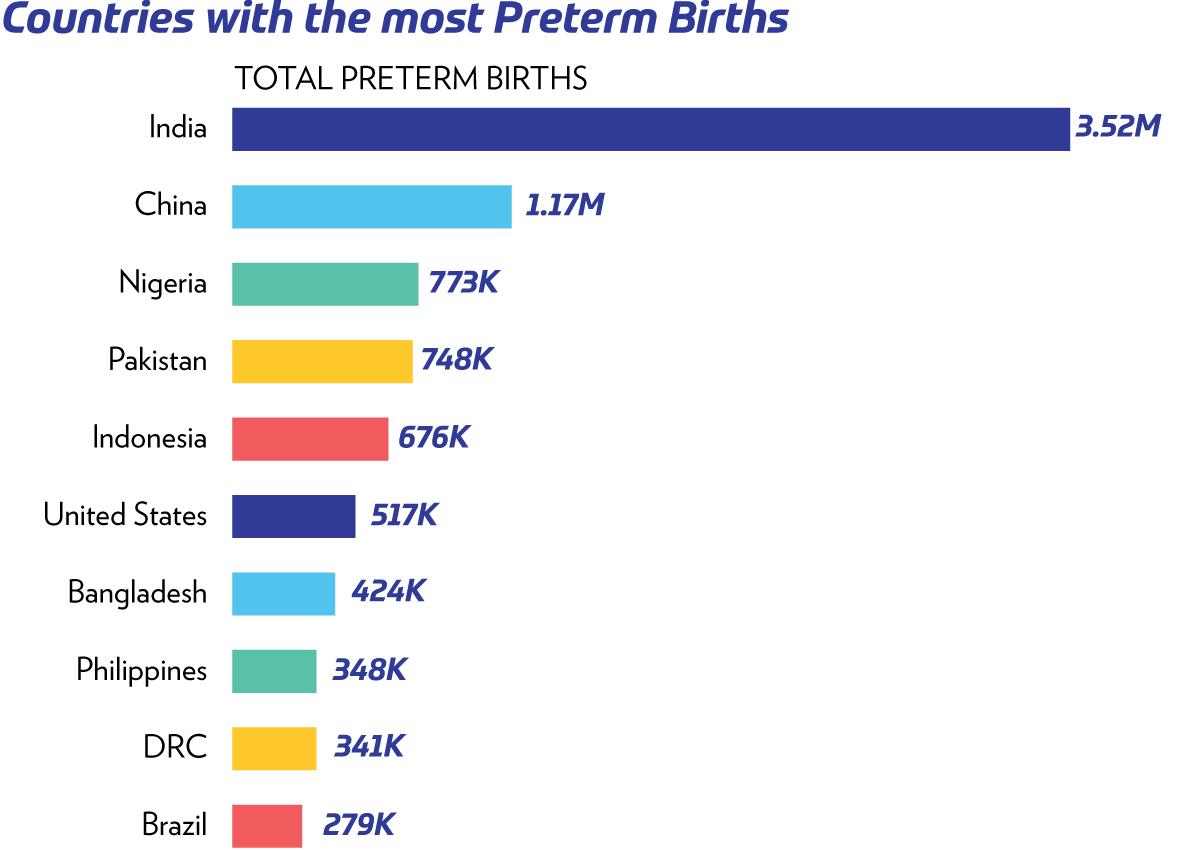
Figure 1: World Health Organization Preterm Birth Statistics | Source
If we can understand and perhaps predict preterm deliveries and stillbirths, perhaps we can prevent them. What data would we need to make sound predictions? What interventions would be necessary to improve health outcomes? It is of high value to identify and refine predictive algorithms for reducing prematurity and stillbirths based on personalization and stratification that goes beyond genomics to incorporate expanded use of the SDOH.
Use Case 1: Pregnancy Risk Factors
In the first approach, a comprehensive view of the pregnancy, from preconception through postpartum periods, both the mother and fetus, are examined in detail in terms of critical decision points and exploring what challenges/questions physicians and patients face along this journey.
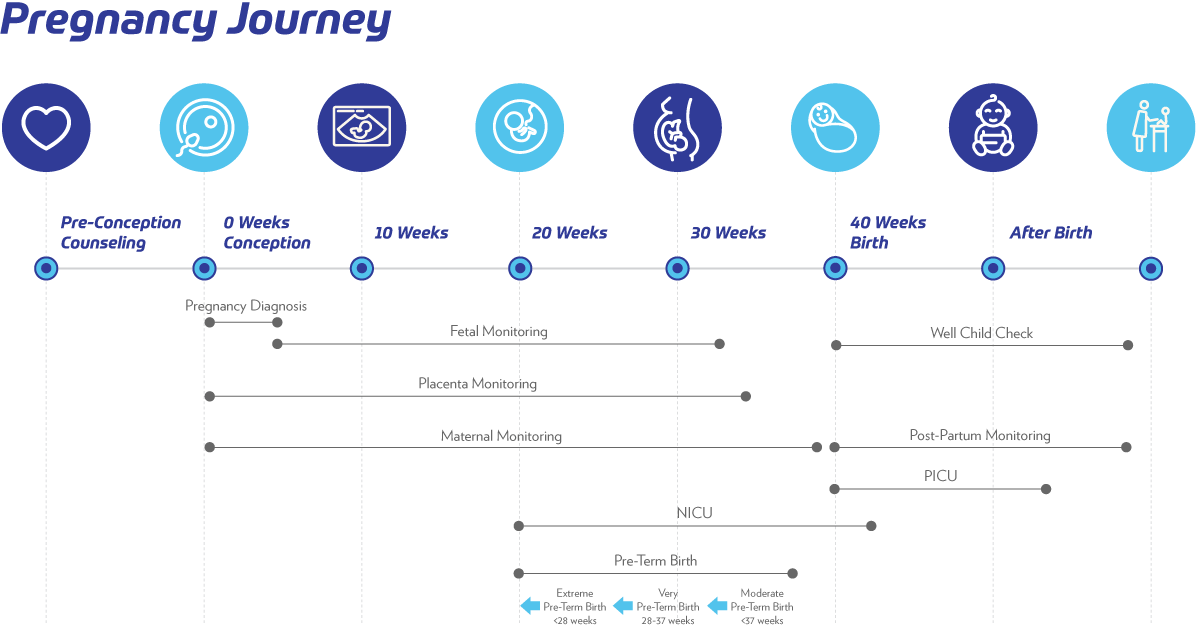
Figure 2: Diagram on Pregnancy as a Set of Processes, Involving the Mother, the Fetus and the Placenta, That Evolve Over Time | Enlarge image
We provide a detailed, integrated roadmap of procedures, testing and evaluations that could comprise an enhanced version of this journey, while recognizing that there are critical factors, involving both social and cultural determinants of health that impact both patients and affect compliance and outcome. This roadmap separately examines the processes involved in preconception counseling, pregnancy diagnosis, maternal/fetal/placental monitoring and postpartum monitoring of mother and child, and identifies both challenges and opportunities for innovation in both concepts and technologies.
These include:
- Need for complex data modeling and data integration of electronic health records (EHRs), medical record coding/billing, registries, health information exchanges (HIEs), public health clinics, lifestyle and environmental data, guidelines and literature within a functional model of pregnancy, e.g., ontologies, knowledge graphs
- Incorporation of temporal data, both cross-sectional and temporal and anticipation of real time, i.e., mobile device, data acquisition and integration, e.g., pattern recognition, inference, addressing missing/conflicting data
- Need to enable complex algorithmic analysis in the background and visualization/presentation of results in a readily digestible manner for physician and patients, e.g., enhanced means for communication, virtual reality
- Ability to detect communities exhibiting similar behaviors, i.e., clinical phenotyping, in high dimensions and using temporal data that are data driven beyond conventional clustering methods, e.g., machine learning, deep learning, quantum computing
- Critical integration of both social and cultural determinants of health to enable more effective translation from public health to personal health, e.g., knowledge graphs, natural language processing (NLP)
- Anticipation of new molecular markers, e.g., microbiome (vaginal, gut, skin), metabolomics, gene/protein expression patterns for impact both preconception and during pregnancy, e.g., ontologies, knowledge graphs
- Monitoring patient adherence to prescribed behavior and physician compliance to guidelines as well as changes in behaviors during pregnancy, e.g., algorithmic development
In Figure 2 we present details of a patient journey along with example pregnancy experiences that women might face as they present in real world practice scenarios.
The Innovation Committee believes that significant contributions to the conception, development, dissemination and implementation of innovative technologies and ideas/approaches can benefit greatly by first starting with better definitions and understanding of the problems/challenges as they exist for the actual members of the healthcare ecosystem.
To accomplish this, the communities need to address the complexity of real-world patients and clinical practice. Also to acknowledge the existence of gaps and conflicts in a transparent manner. This requires approaching critical clinical problems using systems-based and process-based models. This also includes expanding the lens through which these issues are currently addressed. We need to address multivariate factors that define who the patient represents and how they may respond or behave to disparate health experiences and access to digital care.
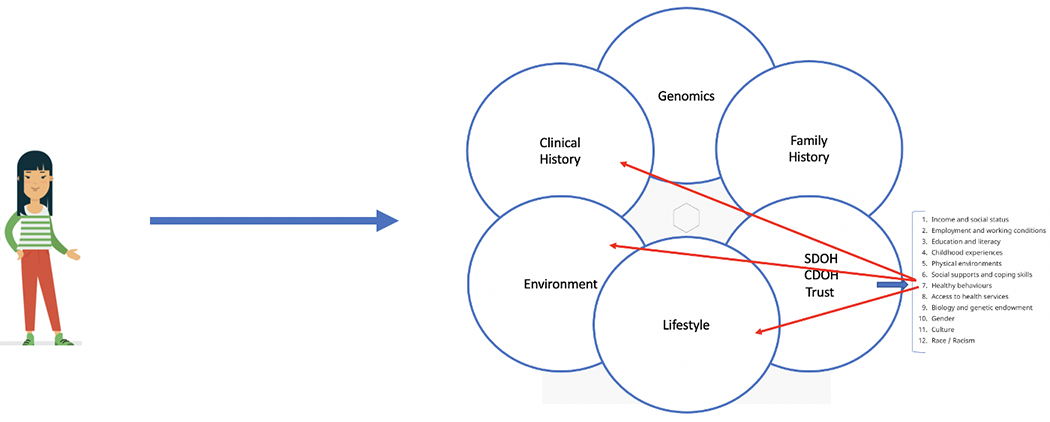
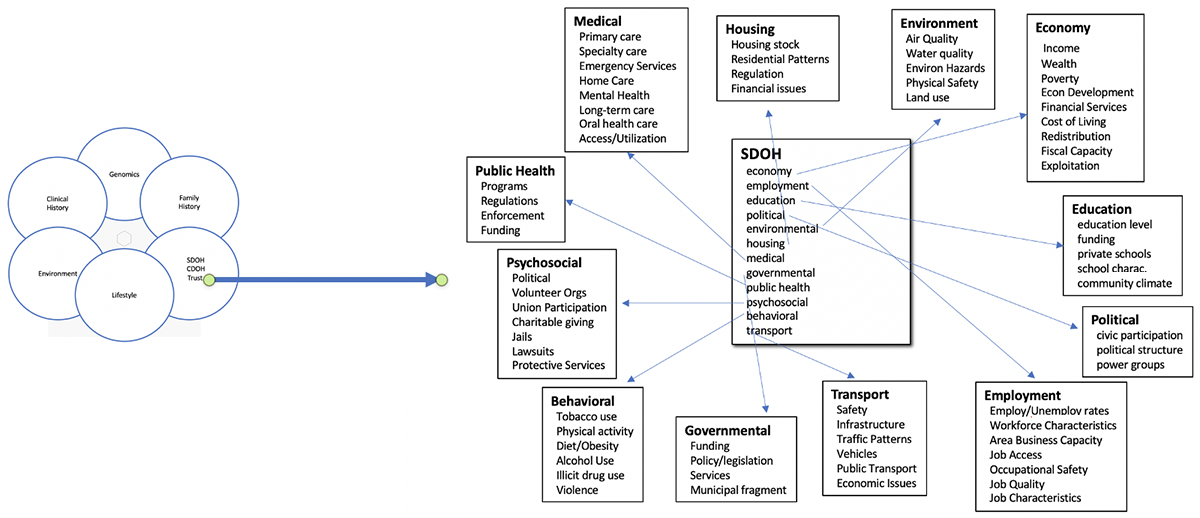
Figure 3: The Complex Factors that Define an Individual | Source: IPQ Analytics | Enlarge image 1 | Enlarge image 2

Table A: Digital Technology Capabilities | Enlarge image
Use Case 2: Preterm Birth
In another approach, specific innovative technology is being used to alert clinicians to the potential onset of preterm labor through monitoring of the mother, and the opportunity to enhance the outcome with more than one in 10 pregnancies with elevated risk of adverse health conditions for mother and/or fetus.
Noninvasive wearable devices that communicate with a smartphone can be combined with machine learning to reassure expectant mothers and provide healthcare providers of maternal care services with better information to improve birth outcomes. This can be achieved through real-time monitoring through a sensor for frequency, regularity and irregularity of contraction patterns also available to the care team, including mother’s blood pressure, fetal movement and heart rate, and other physiological functions. The device(s) can collect and analyze data and communicate with doctors based on notification thresholds.
In motion monitoring of the mother and baby’s heart can provide most critical health parameters of the mother and fetus from conception to birth. This reduces prenatal visits and alerts the doctor to pregnancy complications.
Through machine learning and data collection of large comprehensive datasets on maternal and fetal health, it creates a valuable resource for healthcare providers to identify causes and biomarkers of preterm labor, and also provides detection between labor and false alarms.
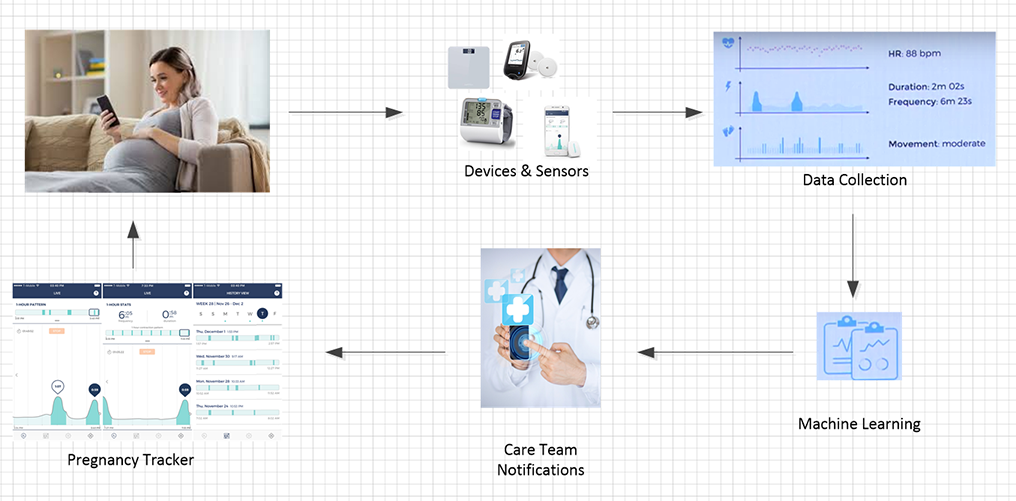
Figure 4: Example Patient Journey | Source: Bloomlife | Enlarge image
This figure depicts integrated systems for healthy pregnancy and early detection of preterm labor. Throughout the patient’s overwhelming biological journey, with enhanced early detection and timely access to care, the innovation can help improve healthcare outcomes for mother and fetus, preventing maternal and neonatal morbidities, and lower cost of healthcare. It serves to help understand how innovation could change the current state experience for early detection/prevention of preterm labor through wearables and real-time data collection with AI/machine learning to identify health risks early and prevent adverse events.
Appendix A
Goal: Develop a process for the HIMSS Innovation Committee to prioritize healthcare system “problems we need to solve” with innovation.
Process:
Step 1: Develop the template for collecting and organizing “problems we need to solve” with innovation.
Step 2: Review template with Innovation Committee members, followed by relevant HIMSS committees
Step 3: Select “problems we need to solve” for sub-work groups to further elaborate and outline innovative solutions.
Step 4: Explore other uses of the template within HIMSS.
Framework: Use the Quadruple Aim categories as the foundation for defining and addressing the “problems we need to solve” with innovation. In recognition of not everything fitting neatly into the Quadruple Aim categories, add additional categories (e.g., research) as needed.
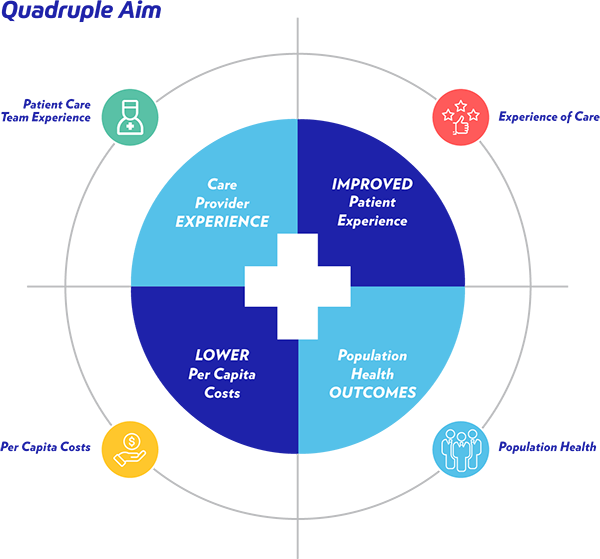
Figure 5: Quadruple Aim | Source
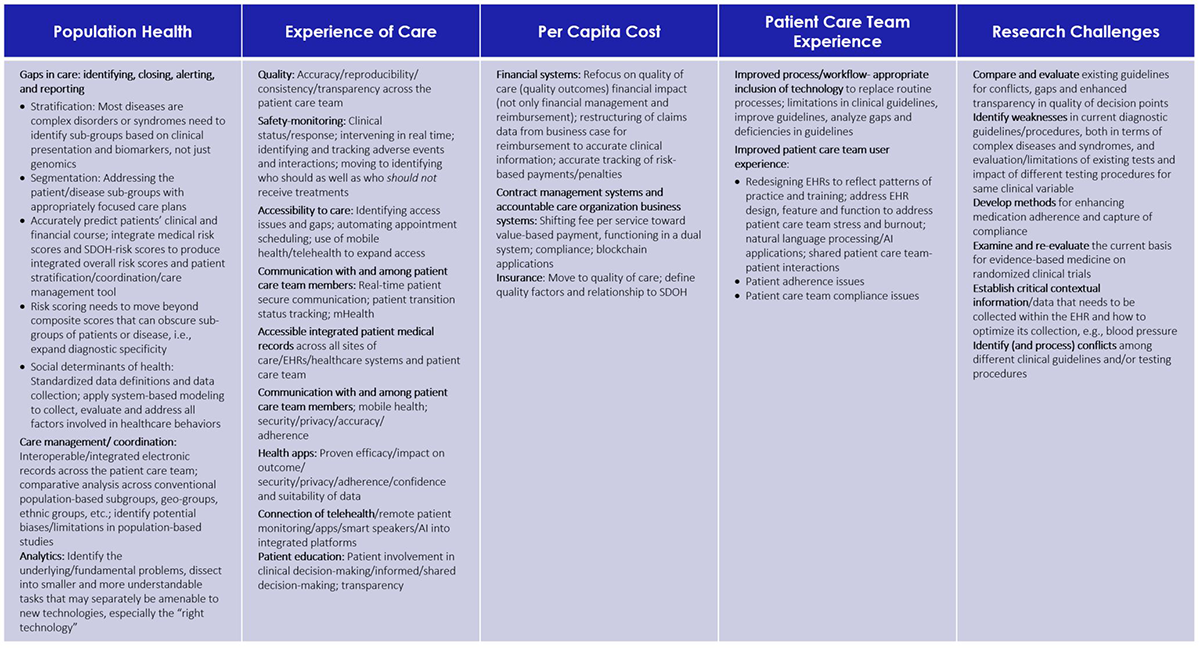
Table B: Quadruple Aim Categories Mapped to Research and Development Use Case Innovation Areas | Enlarge image
Appendix B
Enhanced patient journey through pregnancy along with an example of a patient as they might present in real-world practice.
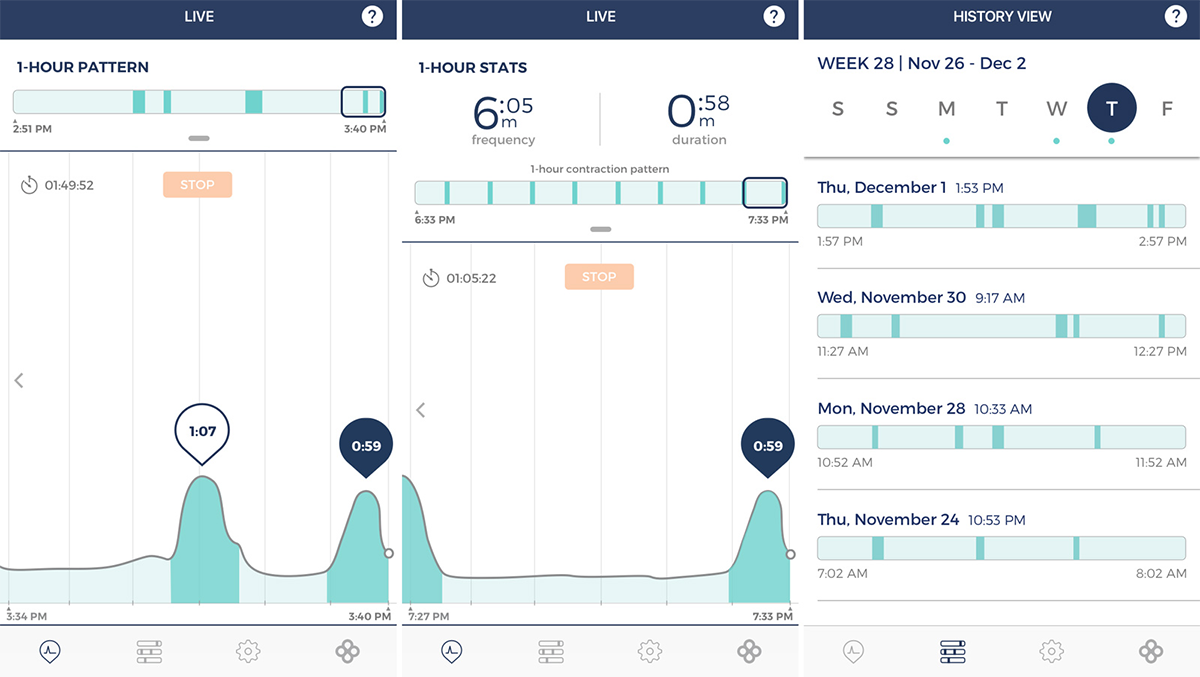
Figure 6: Patient Data Dashboard Collected from Wearable Devices to Assess Progressing Pregnancy | Source: Bloomlife | Enlarge image
Appendix C
A patient care team includes physicians, nurses, advanced practice providers (e.g., APRNs, PAs), and other clinical and non-clinical healthcare workers who provide care.
HIMSS: Driving innovation from the real world
- What are the questions that we would like to answer, independent of whether there is technology or data currently available to answer them
- If we look at available technologies, across all domains, are they:
- Available for implementation today?
- Require adaptation before they can be applied?
- Non-existent and opportunity for development?
- How would you prioritize these questions, or can you?
- Compare these to a real (de-identified) patient journey with current standard of care to highlight gaps and challenges.
The below diagram of the patient journey demonstrates a set of processes for the mother, the fetus and the placenta. Starting at the beginning of the pregnancy journey with Pre-Conception Counseling Follow our case study with Rebecca as it evolves over time with enhanced standards of care.
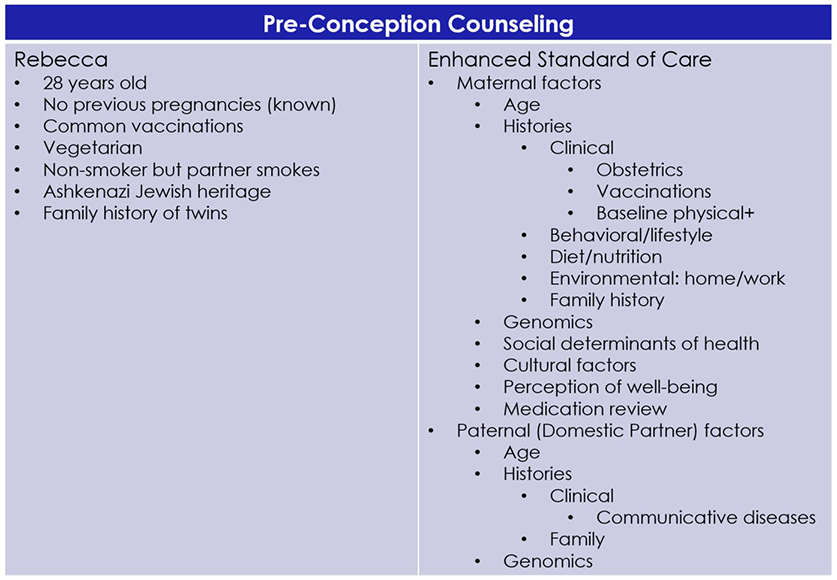
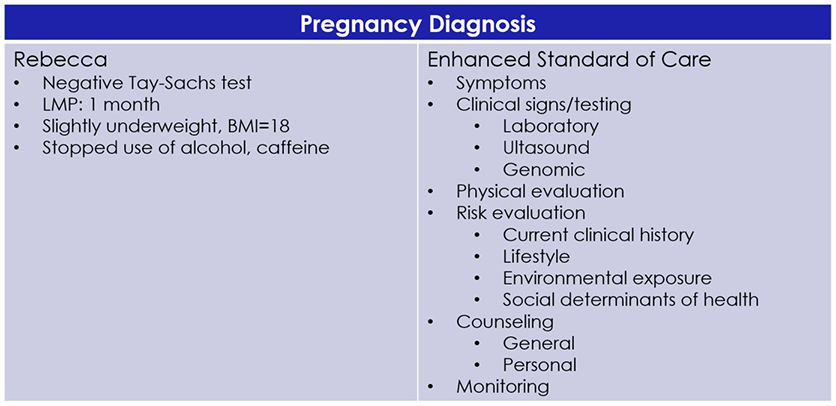
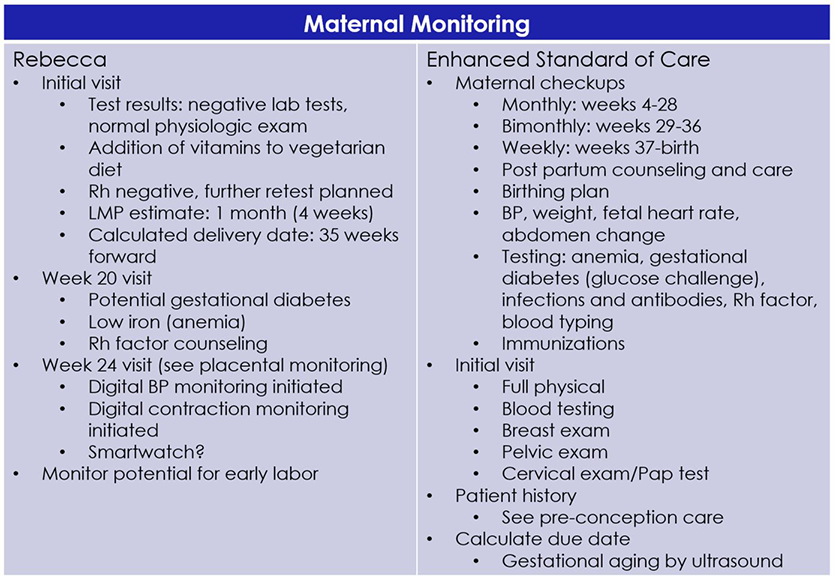
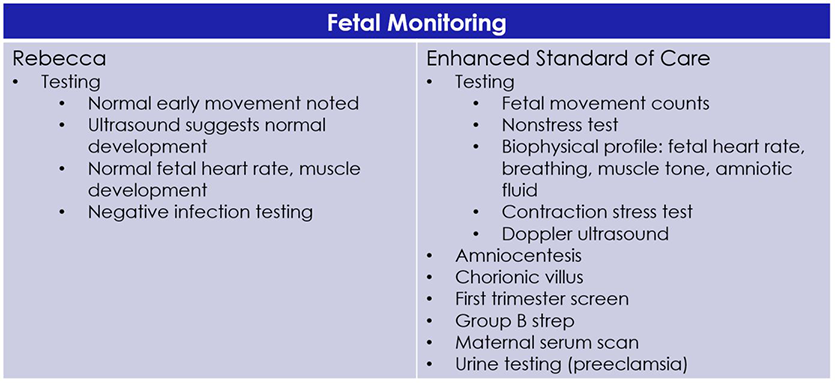
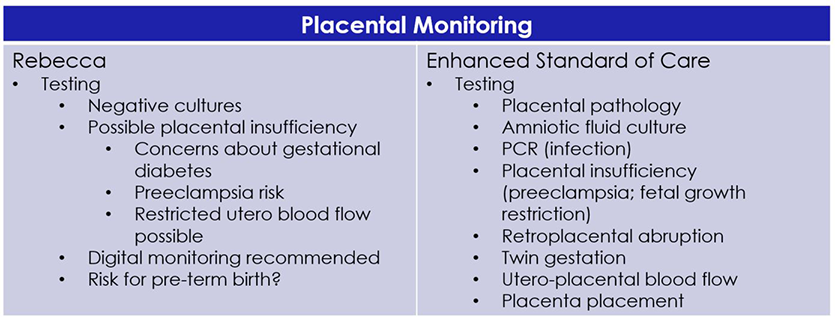
Figure 7: Diagram on Pregnancy as a Set of Processes, Involving the Mother, the Fetus and the Placenta that Evolve Over Time Shown Through Rebecca’s Journey. The Journey Demonstrates the Different Considerations/Questions When Going Through the Patient Journey and Identifies Technologies That Can Inspire Innovation. | Source: IPQ Analytics
Collaborators
- Courtney Baruch Gravett, MPH, Research Program Manager, Global Alliance to Prevent Prematurity and Stillbirths; a HIMSS Collaborator
- Vineet Bhandari, MD, Children's Regional Hospital at Cooper; a HIMSS Collaborator
- Whende Carroll, MSN, RN-BC, Founder, Nurse Evolution; a HIMSS Nursing Informatics Committee Member
- Bonne Farberow , MSN, RN-BC, CCRP, NJ Medical Reserve Corp; a HIMSS Innovation Committee Work Group Member
- William W. Feaster, MD, MBA, Vice President, Chief Health Information Officer, CHOC Children's Hospital; a HIMSS Physician Committee Member
- Joann Imrich, Director, Advanced Analytics, Johnson & Johnson; a HIMSS Innovation Committee Work Group Member
- Kimberly Krakowski, CAHIMS, MSN, RN, Chief Nursing Information Officer, Vice President of Sales, Cipherhealth; a HIMSS Nursing Informatics Committee Member
- Aminkeng Z. Leke, PhD, V. Provost Biaka, University Institute of Buea S.W.R.-Buea Cameroon; a HIMSS Collaborator
- Michael N. Liebman, PhD, Managing Director, IPQ Analytics, LLC; a HIMSS Innovation Committee Work Group Member
- Jim Litch, MD, Executive Director, Global Alliance to Prevent Prematurity and Stillbirths; a HIMSS Collaborator
- Kathleen McGrow, DNP, MS, PMP, RN, Director, Industry Solutions, Microsoft; a HIMSS Nursing Informatics Committee Member
- Owen Montgomery, MD, Gynecology, Thomas Jefferson University School of Medicine; a HIMSS Collaborator
- Anna Panier, CHCIO, FACHE, MBA, Vice President, Integration, Centauri Health Solutions; a HIMSS Innovation Committee Work Group Member
- Amul Patel, Director, Product Integration & Delivery, Health Innovation, Blue Shield of California; a HIMSS Innovation Committee Work Group Member
- David Paul, MD, Christiana Care, Christiana Hospital; a HIMSS Collaborator
- Joel J. Reich, MD, FACEP, CPE, SHIMSS; a HIMSS Innovation Committee Work Group Member
- Jacob Reider, MD, CEO, Alliance for Better Health; a HIMSS Social Determinants of Health Task Force Member
- Jennifer Stoll, Executive Vice President, Government Relations & Public Affairs, OCHIN; a HIMSS Public Policy Committee Member
- Nike Versteegde, MD, Goal3; a HIMSS Collaborator
- Tamara Winden, FHIMSS, MBA, PhD, Chief Research Informatics Officer, Kansas University Medical Center; a HIMSS Public Policy Committee Member
- HIMSS Innovation Committee Members
- HIMSS Nursing Informatics Committee Members
- HIMSS Physician Committee Members
- HIMSS Public Policy Committee Members
We also worked with contacts in the maternal-child health/morality project as well as the menopause transition project, and with groups for all three in Chadighar, India and Shanghai, China and in prematurity and maternal health/mortality in Uganda, Tanzania, Malawi and Algeria. We would also like to thank the HIMSS Innovation Committee for their support.