
Citation: Austin, R., Chi, C., Delaney, C., Kirk, L., Michalowski, M., Pruinelli, L., Rajamani, S., & Monsen K. (2021). COVID-19 response empowered through nursing knowledge generated through existing IT infrastructure. Online Journal of Nursing Informatics (OJNI), 25(1)
Abstract
The current COVID-19 pandemic has created a high demand for an informatics infrastructure to support data interoperability and transparency. The use of the existing infrastructure, Unified Medical Language System (UMLS), supports and promotes informatics practice, research and policy. Nursing informatics should leverage the UMLS resource repository to support quality, effective, person-centric health care and respond to this pandemic. In this paper, we describe the use of UMLS by nursing informaticians through three exemplars to showcase the importance of this resource to advance health and health care, knowledge discovery, and formulate rapid responses to COVID-19. The three exemplars include the Nursing Knowledge Big Data Science Initiative, Omaha System Partnership for Knowledge Discovery and Health Care Quality, and Knowledge Representation of Integrative Health. We include recommendations for future work and policy recommendations to advance interoperability and transparency.
Background
The first version of the Unified Medical Language System (UMLS) was published in 1990 from the National Library of Medicine (NLM) (Bodenreider, 2004; National Library of Medicine, 2019). The UMLS provides resources related to terminologies, vocabularies and coding to facilitate system integration of various terminologies and coding systems (Bodenreider, 2004; National Library of Medicine, 2019). The UMLS consists of three components and includes the metathesaurus, semantic work, and lexicon. The metathesarus includes terms and codes from many vocabularies including the Systemized Nomenclature of Medicine Clinical Terms (SNOMED CT) and Logical Observation Identifiers Names and Codes (LOINC)(National Library of Medicine, 2019). Semantic work consists of categorization of concepts and their relationships within the UMLS, and the lexicon includes tools such as Natural Language Processing (NLP) (National Library of Medicine, 2019). The UMLS brings together health and biomedical vocabularies, including standardized nursing terminologies, to enable interoperability among computer systems. The American Nursing Association (ANA) recognizes 12 standardized nursing terminologies (Table 1) (American Nurses Association, 2018)
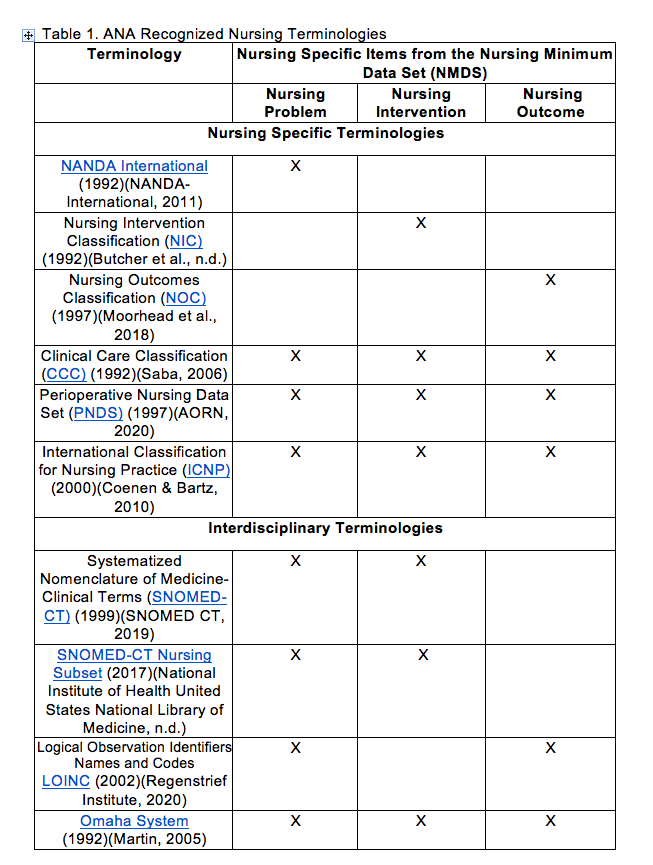
Table 1 ANA Recognized Nursing Terminologies
UMLS has played an integral part in the alignment of nursing terminologies (e.g., Omaha System), has had a profound impact on the field of nursing informatics, and is foundational to big data science in nursing (Coenen et al., 2001; National Institute of Health, National Library of Medicine, n.d.). The latest version of the UMLS (2019AB) includes the following current versions of the ANA-recognized nursing terminologies: NANDA-I (2018 AA), ICNP (2019AB), CCC (2018AA), NIC (2018AB), NOC (2018AB), PNDS (2018AB), and the Omaha System (2007AC). UMLS resources and information are foundational for information structures within the electronic health record (EHR) and for supporting current research and practice to integrate nursing data into clinical data repositories for common data models and for reuse in big data science (Monsen et al., 2016, 2017; National Library of Medicine, 2019; Topaz & Pruinelli, 2017; Westra et al., 2015).
Objective
The purpose of this paper is to describe the use of the UMLS by nursing informaticians through three exemplars that advance health care, knowledge discovery, and responsiveness to COVID-19. The three exemplars from the University of Minnesota Center for Nursing Informatics are aligned with the UMLS and terminology resources and include: 1) Nursing Knowledge Big Data Science Initiative; 2) Omaha System Partnership for Knowledge Discovery and Health Care Quality, and 3) Knowledge Representation of Integrative Health. Further support of this work was evidenced by a preliminary search that resulted in 82 scientific papers published in PubMed related to UMLS and nursing. While not an exhaustive list, this corpus demonstrated the extensive UMLS-related contributions to the science and implementation of standardized nursing terminologies over the last 30 years.
EXEMPLARS
Exemplar 1. Nursing Knowledge Big Data Science Initiative. Now in its eighth year, this initiative aims to develop and advance an action plan for shaping health policy and informatics knowledge discovery based on sharable, comparable nursing data (Delaney & Westra, 2017; UMN Center for Nursing Informatics, 2020; Westra et al., 2015). Hosted by the University of Minnesota Center for Nursing Informatics (UMN), the initiative provides a structure for leaders from various nursing and health sectors including academia, health systems, government institutions, national associations, and software vendors to advance a national plan to capture nursing information for big data research, make progress toward achieving the Institute for Healthcare Improvement’s Quadruple Aim, and improve health outcomes. As a national working conference and year-round working infrastructure, the initiative continues to develop and guide consistent documentation and data collection practices to support nursing big data research for transforming health care. The initiative encompasses workgroups actively advancing the UMLS vision specifically for nursing. The current workgroups span coordination, context of care, data science and clinical analytics, encoding and modeling, e-repository, knowledge modeling, policy and advocacy, mobile health for nurses, nursing informatics education, nursing value, social behavioral determinants of health, and transforming nursing documentation (UMN Center for Nursing Informatics, 2020).
In response to COVID-19, the 2020 working conference shifted to four virtual sessions held from June to September 2020. The focus of the virtual sessions ranged from expanding data-driven COVID-19 best practice discoveries to leveraging nursing big data science. The sessions brought together national leaders from various domains, such as clinical practice, academia and industry perspectives and included breakout rooms to enable discussion between participants. The breakout room discussions provided the opportunity to create a shared understanding of informatics application technologies used during the pandemic. Hosting the working sessions in this format further facilitated conversations related to the current state of big data, the use of real-time data, and the use of big data to support pandemic efforts where appropriate. Furthermore, several working groups shifted the focus toward pandemic support. For example, the Nursing Value Working Group developed methods for measuring nursing contributions to individual patient outcomes and the cost of delivering care from a single nurse perspective (Moon et al., 2019; J. Welton & Harper, 2016, 2017). This value-based financial model integrated Nursing Management Minimum Data Set (NMMDS), SNOMED CT, LOINC, administrative codes, and nursing terminologies including Nursing Intervention Classification (NIC) and Nursing Outcomes Classification (NOC). This workgroup is also working on incorporating artificial intelligence (AI) for better clinical nursing reasoning, a key measure to demonstrate the value of nursing care.
Similarly, the Knowledge Modeling Workgroup developed information models (IMs) derived from EHR flowsheet data and used these IMs to extract clinically useful information from the EHR to advance data science knowledge generation. As a result, an IM for pain was built. The IM pain model has been nationally validated and is linked to LOINC and SNOMED CT (Westra et al., 2018; Westra, Christie, et al., 2017). This approach provided new directions to understand the context within which pain occurs in the management of opioid use, thus supporting the work of the Data Science and Clinical Analytics Workgroup to educate and expand the use of analytics techniques for nursing knowledge generation (Pruinelli et al., 2018, 2020). The process of developing IMs has enabled the workgroup to use this knowledge and apply it to documentation and data sharing during the pandemic.
The initiative also supports a publicly available resource that provides access to all materials developed and shared throughout the last eight years (UMN Center for Nursing Informatics, 2020). A unique communication strategy leveraging the web and LinkedIn functionalities are available for workgroups. This web-LinkedIn tool is a searchable, topic-driven repository for big data articles, workgroup reports, presentations, and other documents. It is paired with a LinkedIn group to allow discussion of posted information on big data topics with colleagues and peers. Members have shared more than 115 publications that showcase the impact of this initiative, with more publications in development and review. Members of the initiative have testified at the National Academies, the World Health Organization, and other policy-setting conferences and organizations. Initiative members engage with other professionals across nursing specialties and with other interprofessional peers and use the UMLS to advance standardized terminologies and promote interoperability.
Exemplar 2. Omaha System Partnership for Knowledge Discovery and Health Care Quality. This partnership is a practice-based research network within the University of Minnesota School of Nursing Center for Nursing Informatics (UMN Center for Nursing Informatics, 2020; Westra et al., 2015). The UMLS metathesaurus lists the Omaha System, a multi-disciplinary standardized interface terminology, as a source vocabulary in the UMLS. The UMLS metathesaurus provides metadata and detailed statistics regarding the counts and distribution of terms, supporting the Omaha System as a known terminology for health and health care (Martin, 2005). This UMLS recognition, foundational for the uptake and use of the Omaha System software in the 1990s continuing to the present, has had a positive impact toward realizing the anticipated and desired goals of practice-generated data being reused to evaluate the quality of care and discover new knowledge. Further, the UMLS SNOMED CT browser enables public searches for Omaha System terms, which are embedded within SNOMED CT and LOINC.
The Omaha System Partnership consists of scientific teams, community partners, and a collaborative of de-identified clinical Omaha System data (Monsen et al., 2012). Researchers and clinicians use these data to generate new clinical knowledge related to health care quality and the health of diverse populations, and to develop new methodologies for reusing standardized clinical data. Findings from this research have implications for clinical practice, research and health policy. Since its inception in 2010, more than 100 partnership studies involving community partners in practice organizations, student investigators, and researchers at numerous institutions in the United States and internationally were completed or are in progress (Monsen et al., 2012; UMN Center for Nursing Informatics, 2020). In response to COVID-19, the partnership launched an international effort to deploy evidence-based guidelines for using the Omaha System to support COVID-19 for disease prevention and control activities and documentation at the individual, family and community levels (Monsen, 2020). This work has resulted in an evidence-based guideline that includes 108 interventions for 45 COVID-19 response roles ranging from community members to acute care providers (Monsen, 2020). The existing infrastructure of the UMLS has been pivotal to the adoption of the Omaha System and will be a key factor in sustaining the growth and impact of partnership research.
Exemplar 3. Knowledge Representation of Integrative Health. As the value of non-pharmacological therapies is increasingly recognized, these therapy modalities need to be represented in standardized terminologies (Clarke et al., 2015; Han et al., 2018; Skelly et al., 2018). During COVID-19, non-pharmacological approaches have been examined to augment current evidence-based guidelines (Alschuler et al., 2020). For example, traditional Chinese medicine (i.e., acupuncture) shows promise as a potential adjunctive therapeutic option to COVID-19 (Chan et al., 2020; Li et al., 2020). As new evidence continues to emerge, it is imperative to document and represent non-pharmacological therapies within the EHR.
Before the pandemic, this interprofessional research team evaluated the representation of non-pharmacologic therapies within the comprehensive international standardized clinical health care terminology, SNOMED CT (SNOMED International, 2019). UMLS was leveraged to examine the non-pharmacological term coverage within SNOMED-CT. This work was performed in response to the opioid epidemic and recommendations from several national organizations on the use of non-pharmacological therapies that found EHRs lacked representation of these therapies (Centers for Disease Control and Prevention, 2017; Cockayne et al., 2005; Joint Commission, 2017, 2018; Porter, 2017; Stan et al., 2018).
A total of 1,209 non-pharmacological therapy terms from multiple selected foundational references and resources in integrative health were extracted (Bauer, 2017; Kreitzer & Koithan, 2019, 2014; Leibowitz & Smith, 2006; Lindquist et al., 2018; National Center for Biotechnology Information National Institute of Health, 2018; National Center for Complementary and Integrative Health (NCCIH) 2019; Wieland et al., 2011). Of the 578 terms validated through consensus, over half (51.9%) of the terms were not found within SNOMED CT. This research was the first step to identify non-pharmacological term coverage within SNOMED CT and, consequently, in the UMLS. The next steps include broad dissemination of these findings with interprofessional organizations and associations (e.g., American Medical Informatics Association (AMIA) and Academic Consortium for Integrative Medicine and Health) to develop consensus for new non-pharmacological terminology content to be included in SNOMED CT. Future research includes analysis of clinical EHR non-pharmacological therapy data to compare with the non-pharmacological therapy terms mapped/non-mapped to SNOMED CT to develop core data elements for use across health care organizations and settings. The team proposes to add a non-pharmacological therapy SNOMED CT subset to existing UMLS resources to ensure consistent use of the existing and new terms. This work has high value given the need for reliable quality evidence-based practices during and after the pandemic.
Discussion
Three UMLS-related exemplars advance the science of nursing informatics to improve health and health care for patients, families, and communities. The University of Minnesota Center for Nursing Informatics leveraged the power of UMLS in the integration of diverse nursing data across settings and stakeholders to support knowledge discovery. As nursing informatics science continues to evolve, the influence and continued support of the UMLS in promoting standardized nursing and interprofessional health care terminologies is essential for advancing national health policy, adoption into EHRs, and use in clinical care. These examples demonstrate the ability to shift the focus to advance health outcomes resulting from the standardization and integration of nursing data, information and knowledge during the pandemic (Bakken, 2020; Monsen, 2020).
We have several recommendations. First, nursing informatics leaders must advocate for the use of standardized terminologies within EHRs through national health policy work by serving as members of task forces on interoperability for quality, consumer data sharing, and national governance structures. For example, in the Nursing Knowledge Big Data Science Initiative and the Omaha System Partnership, nurse informaticians work collaboratively across health organizations, academia, vendors, and national associations on policy recommendations to optimize information systems through the use of data standards that are aligned with the nursing process and support the practical application at the point of care (Delaney & Westra, 2017; Monsen et al., 2012; Westra et al., 2015). Numerous studies conducted by the initiative and partnership demonstrate that it is critical that informatics science and UMLS promote accurate representation of nursing data and work to ensure that the voice of nursing and those that nurses care for – individuals, families and communities – are represented within health data (Gephart et al., 2018; Topaz & Pruinelli, 2017; Westra et al., 2015). Given the importance of representation in health data, a national policy is needed for the adoption and use of standards to occur.
Second, we recommend that health systems and EHR vendors use standardized terminologies in value-based care and population health management solutions (Minnesota Department of Health Office of Information Technology, 2014; Office of the National Coordinator, 2017). The shift toward value-based care underlies the need for structured, interoperable data that can be shared across stakeholders, systems and settings (Centers for Disease Control and Prevention, 2020; Office of the National Coordinator for Health Information Technology, 2020). The UMLS makes sense of this complex environment and promotes interoperability across all systems and platforms, as we described in the non-pharmacological core data elements case study. During this pandemic, nursing informatics experts and researchers are well-positioned to drive this widespread adoption as they understand the value of structure and codification of data in conjunction with nursing information in larger datasets (Bakken, 2020; Chow et al., 2015; Jiang et al., 2017; Topaz & Pruinelli, 2017; Westra, Sylvia, et al., 2017).
Finally, in alignment with the UMLS's stated purpose to "facilitate the development of computer systems that behave as if they ‘understand’ the meaning of the language of biomedicine and health" (National Library of Medicine, 2019, para. 1), we recommend the reuse of standardized data for evaluation and knowledge discovery. Three examples - Nursing Knowledge Big Data Science Initiative, Omaha System Partnership and SNOMED mapping support consistent documentation of the interventions for nursing and all health care roles for future discovery of what worked during the pandemic. This work begins with defining the data elements as described in the non-pharmacological case study exemplar and is advanced through collaboration described in the initiative case study. The partnership case study highlights knowledge and wisdom to improve practice and inform the science through research. Nursing informaticians are committed to leading this work across the health professions to advance the UMLS agenda.
Conclusion
This paper highlights the influence of UMLS in supporting nursing informatics science, specifically during COVID-19. Over the last 30 years, the UMLS has been a shared resource for health and nursing informatics science. Given the current global pandemic, these three exemplars from the University of Minnesota Center for Nursing Informatics illustrate the use of the existing UMLS and showcase the importance of this resource in continued knowledge generation. To further advance the science, we recommend and advocate for nursing terminology standards through national health policy, use of standards in EHRs, and reuse of standardized data for research.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interest statement: The authors have no competing interests to declare.
Contributorship statement: All authors on this manuscript meet the International Committee of Medical Journal Editors’ criteria for authorship.
Acknowledgments: The authors have no acknowledgments to disclose.
Online Journal of Nursing Informatics
Powered by the HIMSS Foundation and the HIMSS Nursing Informatics Community, the Online Journal of Nursing Informatics is a free, international, peer reviewed publication that is published three times a year and supports all functional areas of nursing informatics.
References & Bios
Alschuler, L., Weil, A., Horwitz, R., Stamets, P., Chiasson, A. M., Crocker, R., & Maizes, V. (2020). Integrative considerations during the COVID-19 pandemic. Explore, 16(6), 345–356. https://doi.org/10.1016/j.explore.2020.03.007
American Nurses Association. (2018). Inclusion of recognized terminologies supporting nursing practice within electronic health records and other health information technology solutions. https://www.nursingworld.org/practice-policy/nursing-excellence/officia…
Bakken, S. (2020). Informatics is a critical strategy in combating the COVID-19 pandemic. Journal of the American Medical Informatics Association, 27(6), 843–844. https://doi.org/10.1093/jamia/ocaa101
Bauer, B. (2017). Mayo Clinic Guide to Integrative Medicine. Time Inc. Books.
Bodenreider, O. (2004). The Unified Medical Language System (UMLS): Integrating biomedical terminology. Nucleic Acid Research, 1(32), D267-70. https://doi.org/10.1093/nar/gkh061
Centers for Disease Control and Prevention. (2017). CDC guideline for prescribing opioids for chronic pain — United States, 2016 . Regulatory Alert FDA Warning / Regulatory Alert Recommendations. 65(1).
Centers for Disease Control and Prevention. (2020). Public Health and Promoting Interoperability Programs. https://www.cdc.gov/ehrmeaningfuluse/index.html
Chan, K. W., Wong, V. T., Chi, S., & Tang, W. (2020). COVID-19: An update on the epidemiological, clinical, preventive and therapeutic evidence and guidelines of integrative Chinese – western medicine for the management of 2019 Novel Coronavirus disease. 48(3), 737–762. https://doi.org/10.1142/S0192415X20500378
Chow, M., Beene, M., O’Brien, A., Greim, P., Cromwell, T., DuLong, D., & Bedecarré, D. (2015). A nursing information model process for interoperability. Journal of the American Medical Informatics Association, 22(3), 608–614. https://doi.org/10.1093/jamia/ocu026
Clarke, T. C., Black, L. I., Stussman, B. J., Barnes, P. M., & Nahin, R. L. (2015). Trends in the use of complementary health approaches among adults: United States, 2002-2012. National Health Statistics Reports, 79(79), 1–16. https://doi.org/10.1161/STROKEAHA.113.002813.Oxidative
Cockayne, N. L., Duguid, M., & Shenfield, G. M. (2005). Health professionals rarely record history of complementary and alternative medicines. British Journal of Clinical Pharmacology, 59(2), 254–258. https://doi.org/10.1111/j.1365-2125.2004.02328.x
Coenen, A., McNeil, B., Bakken, S., Bickford, C., & JJ, W. (2001). Toward comparable nursing data: American Nurses Association criteria for data sets, classification systems, and nomenclatures. Computers, Informatics, Nursing : CIN, 19, 240–248.
Delaney, C. W., & Westra, B. (2017). Big Data: Data science in nursing. Western Journal of Nursing Research, 39(1), 3–4. https://doi.org/10.1177/0193945916671687
Gephart, S. M., Davis, M., & Shea, K. (2018). Perspectives on policy and the value of nursing science in a big data era. Nursing Science Quarterly, 31(1), 78–81. https://doi.org/10.1177/0894318417741122
Han, L., Goulet, J. L., Skanderson, M., Bathulapalli, H., Luther, S. L., Kerns, R. D., & Brandt, C. A. (2018). Evaluation of complementary and integrative health approaches among US Veterans with musculoskeletal pain using propensity score methods. Pain Medicine (Malden, Mass.), 90–102. https://doi.org/https://dx.doi.org/10.1093/pm/pny027
Jiang, F., Jiang, Y., Zhi, H., Dong, Y., Li, H., Ma, S., Wang, Y., Dong, Q., Shen, H., & Wang, Y. (2017). Artificial intelligence in healthcare: Past, present and future. Stroke and Vascular Neurology, 2(4), 230–243. https://doi.org/10.1136/svn-2017-000101
Joint Commission. (2018). Joint Commission Enhances Pain Assessment and Management Requirements for Accredited Hospitals. Joint Commission Perspectives, 37(7). https://www.jointcommission.org/assets/1/18/Joint_Commission_Enhances_P…
Joint Commission. (2017). Requirement, Rationale, Reference: Pain Assessment and Management Standards for Hospitals. R 3 Report, 11, 1–7. https://www.jointcommission.org/assets/1/18/R3_Report_Issue_11_Pain_Ass…
Kreitzer, M. J., & Koithan, M. (2019). Integrative Nursing (Second Ed). Oxford University Press.
Kreitzer, M., & Koithan, M. (2014). Integrative Nursing (M. Kreitzer & M. Koithan (eds.); 1st Edition). Oxford University Press.
Leibowitz, R., & Smith, L. (2006). The Duke encyclopedia of new medicine: Conventional and alternative medicine for all ages. Rodale Books International.
Li, Y., Liu, X., Guo, L., Li, J., Zhong, D., Zhang, Y., & Clarke, M. (2020). Traditional Chinese herbal medicine for treating novel coronavirus ( COVID-19 ) pneumonia : protocol for a systematic review and meta-analysis. Systematic Reviews, 9, Article number 75, 1–6.
Lindquist, R. A., Tracy, M. F., & Snyder, M. (2018). Complementary and Alternative Therapies in Nursing (8th Editio). Springer Publishing Company.
Martin, K. (2005). The Omaha System: A Key to Practice. Documentation and Information Management (2nd ed.). Health Connections Press.
Minnesota Department of Health Office of Information Technology. (2014). Recommendations regarding the use of standard nursing terminology in Minnesota. August. https://www.health.state.mn.us/facilities/ehealth/meaningfuluse/index.h…
Monsen, K. A. (2020). Rapid development and deployment of an international Omaha System evidence-vased guideline to support the COVID-19 response. Computers, Informatics, Nursing : CIN, 38(5), 224–226. https://doi.org/10.1097/CIN.0000000000000648
Monsen, K. A., Brandt, J. K., Brueshoff, B. L., Chi, C. L., Mathiason, M. A., Swenson, S. M., & Thorson, D. R. (2017). Social determinants and health disparities associated with outcomes of women of childbearing age who receive public health nurse home visiting services. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing, 46(2), 292–303. https://doi.org/10.1016/j.jogn.2016.10.004
Monsen, K. A., Kapinos, N., Rudenick, J. M., Warmbold, K., McMahon, S. K., & Schorr, E. N. (2016). Social determinants documentation in electronic health records with and without standardized terminologies. Western Journal of Nursing Research, 38(10), 1399–1400. https://doi.org/10.1177/0193945916658208
Monsen, K. A., Martin, K. S., & Bowles, K. H. (2012). Omaha system partnership for knowledge discovery and healthcare quality: Nursing terminology in action. CIN - Computers Informatics Nursing, 30(1), 6–7. https://doi.org/10.1097/NCN.0b013e318245cf3e
Moon, L. A., Clancy, G., Welton, J., & Harper, E. (2019). Nursing value user stories: A value measurement method for linking nurse contribution to patient outcomes. CIN - Computers Informatics Nursing, 37(3), 161–170. https://doi.org/10.1097/CIN.0000000000000520
National Center for Biotechnology Information National Institute of Health. (2018). Complementary Therapies. https://www.ncbi.nlm.nih.gov/mesh/?term=complementary+medicine
National Center for Complementary and Integrative Health (NCCIH). (2019). Complementary, Alternative, or Integrative Health: What’s In a Name? https://nccih.nih.gov/health/integrative-health
National Institute of Health United States Naitonal Library of Medicine. (n.d.). Unified Medical Language System. Nursing Problem List Subset of SNOMED CT. https://www.nlm.nih.gov/research/umls/Snomed/nursing_problemlist_subset…
National Library of Medicine. (2019). Unified Medical Language System (UMLS). https://www.nlm.nih.gov/research/umls/quickstart.html
Office of the National Coordinator for Health Information Technology. (2020). Health IT Legislation. https://www.healthit.gov/topic/laws-regulation-and-policy/health-it-leg…
Office of the National Coordinator. (2017). Standard Nursing Terminologies: A Landscape Analysis. U.S. Department of Health and Human Services. https://www.healthit.gov/sites/default/files/snt_final_05302017.pdf
Porter, L. (2017). National Pain Strategy - A Comprehensive Population Health -Level Strategy for Pain. https://iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508…
Pruinelli, L., Johnson, S. G., Fesenmaier, B., Winden, T. J., Coviak, C., & Delaney, C. W. (2020). An applied healthcare data science roadmpa for nursing leaders: A workshop development, conceptualization, and application. CIN: Computers, Informatics, Nursing. https://doi.org/doi: 10.1097/CIN.0000000000000607
Pruinelli, L., Ma, S., Westra, B. L., Johnson, S. G., O’Conner Von, S., & Speedie, S. M. (2018). Multiple factors drive opioid prescribing at the time of discharge. AMIA ... Annual Symposium Proceedings. AMIA Symposium, 2018, 916–921.
Reeves, J. J., Hollandsworth, H. M., Torriani, F. J., Taplitz, R., Abeles, S., Tai-Seale, M., Millen, M., Clay, B. J., & Longhurst, C. A. (2020). Rapid response to COVID-19: Health informatics support for outbreak management in an academic health system. Journal of the American Medical Informatics Association, 27(6), 853–859. https://doi.org/10.1093/jamia/ocaa037
Skelly, A. C., Chou, R., Dettori, J. R., Turner, J. A., Friedly, J. L., Rundell, S. D., Fu, R., Brodt, E. D., Wasson, N., Winter, C., & Ferguson, A. J. R. (2018). Noninvasive nonpharmacological treatment for chronic pain: A systematic review. 209. https://doi.org/10.23970/AHRQEPCCER209
SNOMED International. (2019). SNOMED CT. snomed.org
Stan, D. L., Wahner-Roedler, D. L., Yost, K. J., O’Byrne, T. J., Branda, M. E., Leppin, A. L., & Tilburt, J. C. (2018). Absent and discordant electronic health record documentation of complementary and alternative medicine in cancer care. The Journal of Alternative and Complementary Medicine, 24(9–10), 988–995. https://doi.org/10.1089/acm.2018.0141
Topaz, M., & Pruinelli, L. (2017). Big Data and Nursing: Implications for the Future. Studies in Health Technology and Informatics, 232, 165–171. https://doi.org/10.3233/978-1-61499-738-2-165
UMN Center for Nursing Informatics. (2020). Nursing Knowledge: Big Data Science. https://www.nursing.umn.edu/centers/center-nursing-informatics/news-eve…
Welton, J., & Harper, E. (2017). Case study 5.1 Value-based nursing care model development. In Big Data-Enabled Nursing: Education, Research, and Practice (pp. 95–101). Springer International Publishing.
Welton, J. M., & Harper, E. M. (2016). Measuing Nursing Care Value. Nursing Economics, 34(1), 7–16.
Westra, B. L., Christie, B., Johnson, S. G., Pruinelli, L., La Flamme, A., Sherman, S. G., Park, J. I., Delaney, C. W., Gao, G., & Speedie, S. (2017). Modeling flowsheet data to support secondary use. CIN - Computers Informatics Nursing, 35(9), 452–458. https://doi.org/10.1097/CIN.0000000000000350
Westra, B. L., Johnson, S. G., Ali, S., Bavuso, K. M., Cruz, C. A., Collins, S., Furukawa, M., Hook, M. L., Laflamme, A., Lytle, K., Pruinelli, L., Rajchel, T., Settergren, T. T., Westman, K. F., & Whittenburg, L. (2018). Validation and Refinement of a Pain Information Model from EHR Flowsheet Data. Applied Clinical Informatics, 9(1), 185–198. https://doi.org/10.1055/s-0038-1636508
Westra, B. L., Latimer, G. E., Matney, S. A., Park, J. I., Sensmeier, J., Simpson, R. L., Swanson, M. J., Warren, J. J., & Delaney, C. W. (2015). A national action plan for sharable and comparable nursing data to support practice and translational research for transforming health care. Journal of the American Medical Informatics Association, 22(3), 600–607. https://doi.org/10.1093/jamia/ocu011
Westra, B. L., Sylvia, M., Weinfurter, E. F., Pruinelli, L., Park, J. I., Dodd, D., Keenan, G. M., Senk, P., Richesson, R. L., Baukner, V., Cruz, C., Gao, G., Whittenburg, L., & Delaney, C. W. (2017). Big data science: A literature review of nursing research exemplars. Nursing Outlook, 65(5), 549–561. https://doi.org/10.1016/j.outlook.2016.11.021
Wieland, L., Manheimer, E., & Berman, B. M. (2011). Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration. Alternative Therapies in Health and Medicine, 17(2), 50–59. https://doi.org/10.1016/j.biotechadv.2011.08.021.Secreted
Author Bios
Robin R. Austin, PhD, DNP, DC, RN-BC, is an assistant professor at the University of Minnesota School of Nursing and graduate faculty member in the Earl E. Bakken Center for Spirituality and Healing. Dr. Austin integrates her clinical background with informatics methods to represent the patients’ perspective across the health care continuum. She is the co-director of the Omaha System Partnership through the University of Minnesota School of Nursing Center for Nursing Informatics. Through her research, Dr. Austin seeks to empower individuals using technology and include their voice in person-centered care.
Chih-Lin Chi, PhD, MBA, studied health informatics, computer science, and operations research (specializing in advancing informatics tools to promote personalized health care). His research focuses on personalized health management and translational research starting from knowledge discovery from diverse types of data (electronic medical records, claims data, clinical trial data, Omaha system data, long-term patient cohort, omics data, virtual patient data, and other types of data that fit the research purpose) to clinical usage. He has developed several integrative approaches (including clinical trial simulation, machine learning, optimization, artificial intelligence, and clustering analysis) to extract knowledge and evidence from the data to support diverse personalized health care decisions. Specifically, his current research studies include individualizing prediction of long-term cognitive changes in dementia, personalized statin treatment plan to minimize intolerance, optimal individualized anti-clotting treatment plan to minimize risks, individualizing nursing care plans to improve quality and resource-usage efficiency, and identification of metabolomics.
In 2013, Dr. Chih-Lin Chi joined the University of Minnesota as a core faculty member in the Institute for Health Informatics and assistant professor in the School of Nursing. He received his BS and MBA in Taiwan, and PhD in health informatics from the University of Iowa. He completed his postdoctoral training at the Center for Biomedical Informatics, Harvard Medical School, in 2013, focused on translational research.
Connie W. Delaney, PhD, RN, FAAN, FACMI, serves as Professor and Dean, University of Minnesota School of Nursing, and is the knowledge generation lead for the National Center for Interprofessional Practice and Education. She served as associate director of the Clinical Translational Science Institute –Biomedical Informatics, and acting director of the Institute for Health Informatics in the Academic Health Center from 2010-2015. She serves as an adjunct professor in the faculty of medicine and faculty of nursing at the University of Iceland, where she received the doctor scientiae curation is honoris causa (honorary Doctor of Philosophy in nursing) in 2011. Delaney is the first fellow in the College of Medical Informatics to serve as a Dean of nursing. Delaney was an inaugural appointee to the USA Health Information Technology Policy Committee, Office of the National Coordinator for Health and Information Technology, and Office of the Secretary for the U.S. Department of Health and Human Services (HHS). She is an active researcher in data and information technology standards for nursing, health care, and interprofessional practice and education; big data science; and integrative informatics. She serves on numerous health, business/industry, and policy boards/advisory committees. Delaney currently serves as president of FNINR and vice-chair of CGFNS, Inc. She holds a BSN with majors in nursing and mathematics, MA in nursing, and PhD in educational administration and computer applications. She pursued postdoctoral study in nursing and medical informatics, and graduate study in integrative health and healing.
Laura Kirk, PhD, RN, is an assistant professor in the University of Minnesota School of Nursing, with a Bachelor of Science in nursing, a Master of Science in nursing with a focus in community health/long-term care and a minor in gerontology, and a PhD in nursing. Dr. Kirk is a veteran at the University of Minnesota, having completed both undergraduate and graduate studies here over the last 20 years. She is currently involved in research examining the feasibility and efficacy of aerobic exercise interventions on cognition, physical health and function, and psycho-social well-being in older adults across care settings.
Martin Michalowski, PhD, is an assistant Professor in the Population Health Systems Cooperative Unit at the University of Minnesota School of Nursing. His academic background is in computer science and engineering. He graduated from the University of Minnesota with a bachelor’s degree in Computer Engineering. He obtained master’s and doctoral degrees in computer science (with a focus on automated reasoning) from the Information Sciences Institute at the University of Southern California. His research interests lie in using artificial intelligence to support evidence-based patient management and shared decision-making. For the past seven years, he has been working to improve multi-morbid patient outcomes using population-based clinical practice guidelines at the point of care. He also has an entrepreneurial spirit, having co-founded several companies both in health and non-health areas.
Lisiane Pruinelli, PhD, RN, FAMIA, is an assistant professor at the University of Minnesota School of Nursing. She earned a BSN, a teaching degree, a Master of sciences from the Federal University of Rio Grande do Sul, Brazil (she is originally from Brazil), and a PhD from the University of Minnesota. She collaborates with several multidisciplinary projects nationally and internationally to advance nursing informatics worldwide.
Sripriya Rajamani, MBBS, PhD, MPH, FAMIA, is a clinical associate professor at the University of Minnesota School of Nursing. Her multi-disciplinary background includes training in biomedical informatics, public health and clinical medicine. Her research interests include public health informatics, the impact of information technology in public health practice and population health, adoption and use of standards, and measuring and understanding the impact of interoperability. Dr. Rajamani is also a practicing public health informatician with the Minnesota Department of Health and is involved with Minnesota e-health initiatives.
Karen A. Monsen, PhD, RN, FAMIA, FAAN, is a professor at the University of Minnesota School of Nursing, chair of the Population Health and Systems Cooperative, and director of the Center for Nursing Informatics, where she coordinates the doctor of nursing practice nursing informatics specialty. She is affiliate faculty at the university’s Institute for Health Informatics, faculty in the Department of Computer Science and Engineering, and scientific review team member of the National Center for Interprofessional Practice and Education. She directs the Omaha System Partnership, an interprofessional practice-based research network, within the Center for Nursing Informatics. Her career is dedicated to advancing informatics across all professions, and to reusing data to improve health care quality and population health. Her research demonstrates that it is possible to translate interprofessional evidence into practice and to incorporate practice-based evidence from large practice-based datasets using exploratory research methods. She has received numerous awards for her extensive contributions in research, education and service.