
Executive Summary
Local Problem
To decrease the variability in care delivery to improve the standard of care and the outcomes of the patients undergoing a cesarean section (C-section) procedure. Baptist Health South Florida’s (BHSF) Homestead Hospital implemented electronic order sets (PowerPlans ™) in 2017 for the patient population, and over time has improved the length of stay (LOS) and maintained zero maternal deaths and zero venous thromboembolisms (VTEs). Homestead also initiated an enhanced recovery after surgery (ERAS) pilot for the cesarean section population. The goal of the ERAS c-Section pilot was to serve as an adjunct to current practices geared to deliver a multidisciplinary approach to care with a defined multimodal perioperative care pathway designed to reduce the stress response to surgery and accelerate the patient’s recovery. This encompassed people, process and technology as change management impacted the way Homestead Hospital delivered care along with the build and design of the electronic healthcare record (EHR) requirements. The ERAS pilot will be discussed in more detail under the Clinical Transformation section as an example of pending development and redesign. Analytics measuring the utilization of the PowerPlans supported the measurement of adherence to the standard of care compliance and improved outcomes with a decrease in LOS. The overall LOS for the patient population with the implementation of the PowerPlan decreased from 3.0 days in FY 2017 to 2.30 days in 2020 pre-COVID-19. There is a slight increase noted in LOS in Q1 2020.
Key Stakeholders
Physicians, nursing, pharmacy, lactation team, discharge planning, informatics and patients/family.
Technology
EHR data, clinical decision support alerts (e.g., allergies, sepsis, VTE prevention and fetal demise), PowerPlans for bundle compliance, device integration for vital signs and fetal monitoring, bedside specimen collection and scanning, human milk and formula management and analytics for process and outcomes measurement.
People and Process
Physician and staff buy-in, patient counseling, education and commitment pre-op and post-op; ongoing care team education and commitment to care redesign; neonatal bonding, comfort, feeding, safety and discharge follow-up plan.
Lessons Learned
- Buy-in is key for both the care team and the patient and family
- Education of the PowerPlans and ERAS Pathway is a huge key to success
- Sharing analytics to high-light improvements will help keep the process successful
- The build and design of the EHR tools to support the workflow will assist with compliance
- Neonatal components including safety and comfort will help decrease stress of the mother and support a reduced stress response
Define the Clinical Problem and Pre-Implementation Performance
Childbirth is one of the leading causes of hospital admission in the United States and there is documented evidence of variation in C-section rates, costs and outcomes due to variation in care delivery models. BHSF partnered with Navigant on the T2020 initiative which includes redesigning care for select diagnosis related groups. Navigant and the organization decided upon a structure of an OB/GYN Steering Committee as well as a design team. Both teams included representation from the facilities that provide obstetrical care throughout the health system.
The Steering Committee elected to focus on the cesarean section population to improve overall outcomes, including decreased LOS and bundle compliance. The design team collaborated on creating clinical specifications to ensure every obstetric patient get the same care, every time. Initiatives included a decrease in the LOS and overall improved standardization of care. This case study will focus on the implementation of the PowerPlan and compliance in the utilization.
Perinatal Services also participated in the ERAS pilot for elective C-section patients, which decreased the average LOS, reduced the use of opioids for pain among patients and an improved the infection rate. LOS for ERAS patients as compared to non-ERAS was 1.98 vs. 2.29 for the study period. Non-Opioid use in ERAS patients was 80% and use of non-opioids in non-ERAS patients was 37.74%. The surgical infection rate for the ERAS patients was 0% and non-ERAS was as high as 6.25%. Pain control was also 17% better for the ERAS patients. These indicators show evidence that support the improvements made in the pilot study for the cesarean section ERAS patients and will be the subject of the next phase of work.
The overall LOS for the C-section population with improved bundle compliance decreased from 3.0 days in FY 2017 to 2.30 days in FY 2019 and prior to COVID-19 in Q1 2020. Perinatal Care Quality Measures also include standardization practices such as prophylactic antibiotics, VTE prevention and pain control.
The numerators in this case study are the clinical practice being measured for compliance (PowerPlans) and the LOS for the population. The denominator is the patient population which meets the Medicare Severity Diagnosis Related Groups (MS-DRG) definition for C-section cases. Exclusions include hospice, rehab and expired patients. The organization follows the guidelines and recommendations of The American College of Obstetricians and Gynecology (ACOG), CMS, MS-DRG and benchmarks against Premier. Targeted performance (Premier benchmark) is cesarean section LOS of 2.81, Premier bundle compliance of 80% and zero serious safety evens.
Design and Implementation Model Practices and Governance
BHSF’s evidence-based clinical care (EBCC) initiative is a strategic system-wide standardization effort to reduce variation and unnecessary costs while focusing on evidence-based, quality care. The process is driven by key stakeholders and is supported by real-time, statistically supported benchmarked data. The charter was signed in 2016 and provides the foundation for a methodical approach to improve patient outcomes (Figure 1).

Source: Baptist Health South Florida
The methodology begins with a call to action to for an evidenced based care assessment of current and future state, design plan, team approval, development of an implementation plan, measurement and sustainment plans (Figure 2).

Source: Baptist Health South Florida
Each specific project is supported by a sub-group who are experts in on the focus topic. The Service Line Collaborative includes:
- Cardiac and Vascular
- Critical Care
- Emergency Department
- Gastrointestinal
- Hematology
- Infectious Disease
- Neonatology
- Nephrology
- Neuroscience
- OB/GYN
- Oncology
- Orthopedics
- Pharmacy
- Pulmonary
- Sepsis
- Surgery/PEI/ERAS/NSQIP
The organization has partnered with Navigant on the T2020 initiative which includes redesigning care for select diagnosis related groups. They decided upon a structure of an OB/GYN Steering Committee as well as a design team. Both steering and design teams included member representation from the facilities that provide obstetrical care throughout the system. The steering committee elected to focus on the primary patient population having the largest impact in reducing the overall C-section rate at BHSF. The design team collaborated on creating clinical specifications to ensure obstetric patients get the same care every patient, every time. While the work is still underway to decrease the overall cesarean section rate, the team has successfully decreased the overall LOS for the patient population and instituted a pilot for the utilization of Enhanced Recovery after Surgery (ERAS).
Technologies include EHR data, CDS–alerts such as allergies, sepsis and fetal demise, PowerPlans for bundle compliance, device integration for vital signs and fetal monitoring, bedside specimen collection and scanning, human milk and formula management and analytics for process and outcomes measurement. The PowerPlans were rolled out in 2017 and followed the recommendations from ACOG.
Education was completed via lunch and learns with classroom time, on-line formats on the EBCC website via the intranet and on the Baptist Health South Florida website which is available in the public domain. PowerPlan education is a consistent part of physician education and CME education is available with every MS-DRG or pathway as it rolls out. The education for the ERAS C-section pilot began in December 2018 and the first ERAS patient plan of care was started in January 2019. Other facilities along with BHSF followed the piloted plan of care and additional rollouts are expected. As a recommendation of The Joint Commission, the organization also will begin SIM training for maternal hemorrhage and hypertensive crisis.
The vaginal and C-section delivery steering committee meets monthly and consists of representatives from the EBCC, physicians (CMO), nursing leadership, L&D, HIT, AVP neonatal services, perinatal services and clinical education.
Clinical Transformation enabled through Information and Technology
In November 2017, BHSF implemented the PowerPlans to decrease variation in the care of the C-section patient population. Three key areas of focus for decreasing the LOS in the cesarean section population for Homestead Hospital include the prevention of infection, the prevention of deep vein thrombosis and adequate pain control. Evidence based care practices support the implementation of these key elements as part of the standardized process of care to decrease the overall LOS. In addition to the PowerPlans to minimize the variation in care delivery order sets, the team also focused on education of the PowerPlans early rounding to assess the day before expected discharge and accountability, and in January of 2019, Homestead Hospital initiated a pilot for ERAS in a subset of cesarean section patients. The change in care delivery regarding ERAS and those outcomes will drive the next phase of care delivery and expand to a broader base. Once COVID-19 initiatives begin to fall into place, resources can shift back to these types of projects.
PowerPlans that currently exist for C-section include (Figure 3):
- EBCC anesthesia pre-cesarean
- EBCC anesthesia post-cesarean
- EBCC OB L&D cesarean delivery pre-operative
- EBCC OB postpartum cesarean delivery admission

Source: Baptist Health South Florida
PowerForms™ are used by providers to document the data of the cesarean section delivery. This is extractable data and is pulled into the provider’s note which improves the communication of care for the care team (figure 4).

Source: Baptist Health South Florida
Integration remains seamless, as while in the OR patients are associated to the anesthesia vital sign monitors and vital signs interface into the surgical anesthesia module. All documentation takes place in the anesthesia module and once saved creates a document which is visible within the EHR. All medications and fluids administered while in the OR also display in the patient’s eMAR (Figure 5).

Source: Baptist Health South Florida
Other safety aspects include the integration with fetal monitoring. Patients are associated to fetal monitors using the Fetalink™ application. Maternal vital signs interface into PowerChart IView™ in addition to all annotations documented within the Fetalink application. Once the patient is in Post-Anesthesia Care Unit (PACU) the patient is then associated to the bedside vital sign monitors using the associate device function in IView™ where vital signs are also interfaced. Maternal previous C-section history status displays within the Fetalink application in addition to gravida and para counts. Providers are also able to view fetal strips remotely using the Fetalink mobile app, Fetalink+. Any previously saved fetal strips archived throughout patient's pregnancy and can be viewed straight from the Fetalink application as well as within the Women's Health Overview component (Figure 6).
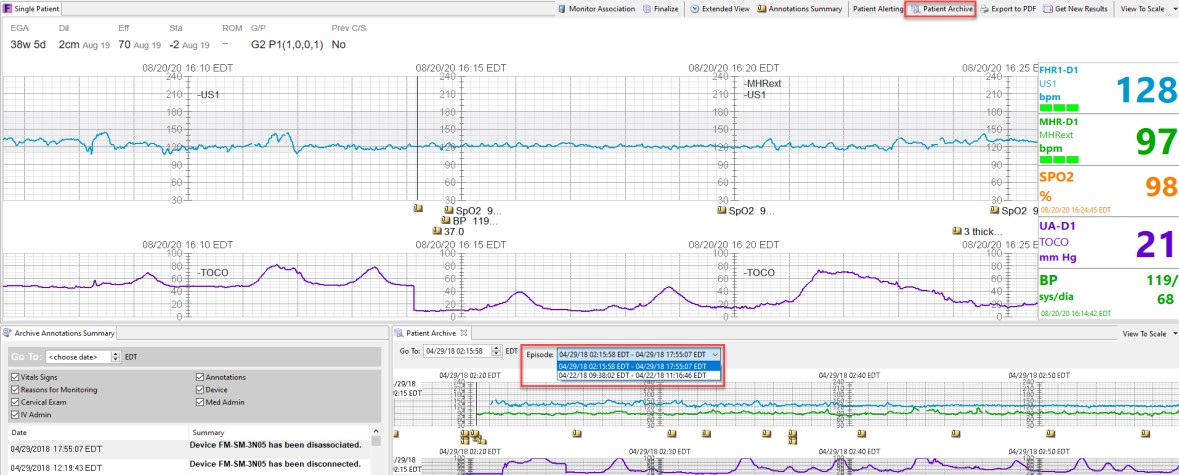
Source: Baptist Health South Florida
Alerts are visible on monitors, dashboards and within the EHR. CDS alerts such as sepsis with the St. John’s sepsis algorithm, allergies, contraindicated medications, weights and even fetal demise are examples of the alerts firing in real-time to keep mother and baby safe (Figure 7).

Source: Baptist Health South Florida
Rounding out the technologies is the capability for bedside scanning for blood, human milk and specimen collection (Figure 8).
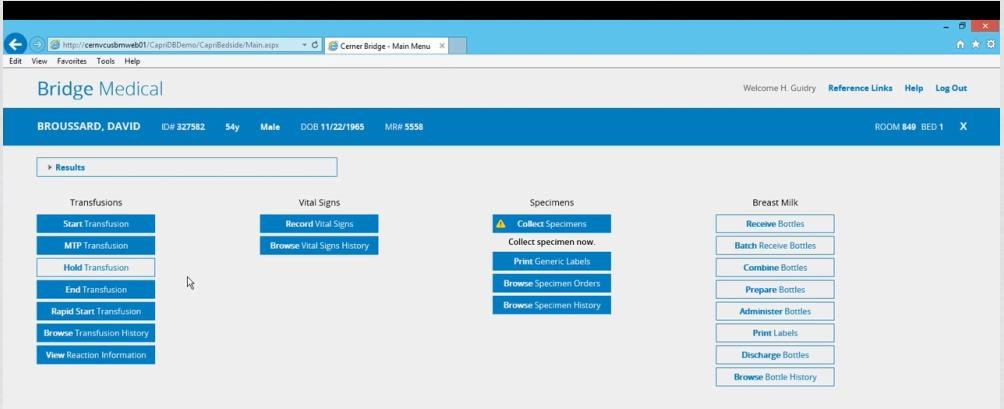
Source: Baptist Health South Florida
People, processes and technology are all important factors in maintaining the safest level of care in the maternal health space. There are many moving pieces and parts, so a fully integrated EHR system increases the ease of use, adoption and standardization of care. The use of evidence based clinical care, tracked with near-real-time analytics helps to ensure improved outcomes such as decreased LOS and decreased safety events such as VTEs and maternal mortalities.
Workflows are mapped out by the interdisciplinary teams and changes are addressed as needed. Clinical decisions and updates to the evidence follow the charter for the EBCC (Figure 9).
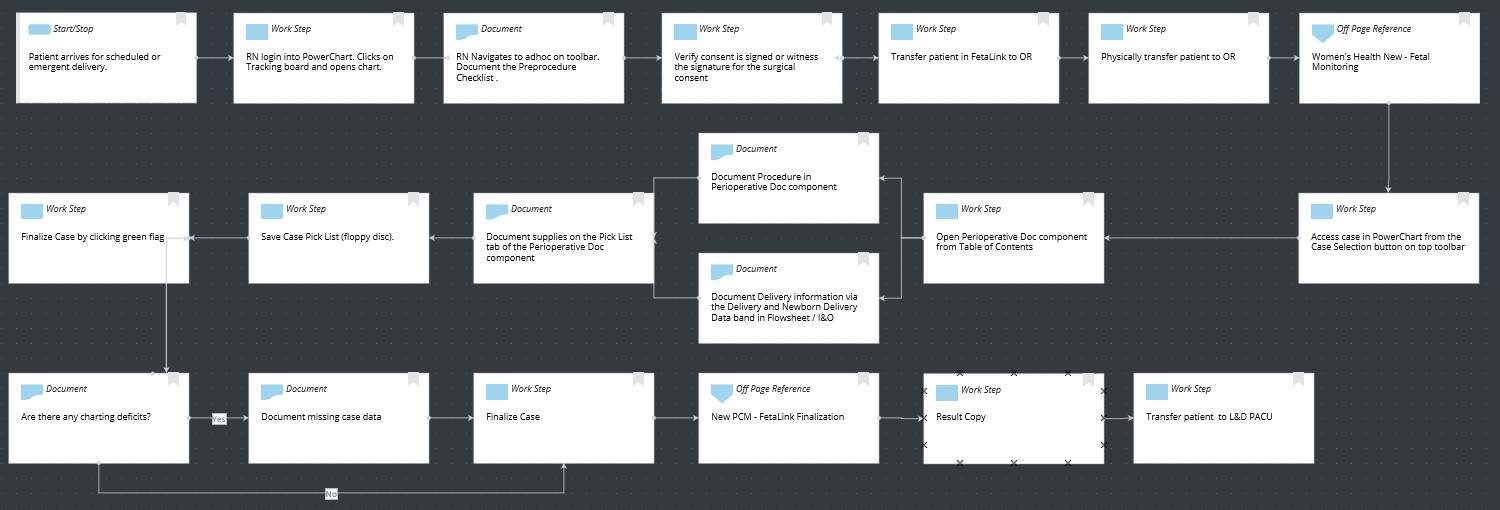
Source: Baptist Health South Florida
Improving Adherence to the Standard of Care
Homestead Hospital, as part of the BHSF care initiatives instituted Power Plans™ to drive the utilization of C-section care bundles to decrease variation of care delivery and improve outcomes for the patient population. Targeting LOS was one of the focus areas with most documented resources support the average hospital LOS post cesarean section to be 2– 4 days. The standardized approach for the PowerPlan rollout, the established educational process and the existing commitment to standardized care via the EBCC structure led to the success of the rollout from the beginning.
The numerator in their care bundle utilization is the clinical practice being measured for compliance (PowerPlan utilization) and the patient population is the denominator which meets the MS-DRG definition for cesarean section cases. BHSF and Homestead Hospital follow the guidelines and recommendations of ACOG, CMS, MS-DRG and benchmarks against Premier. Targeted performance LOS of 2.30 days and bundle compliance of 80% (Figure 10).
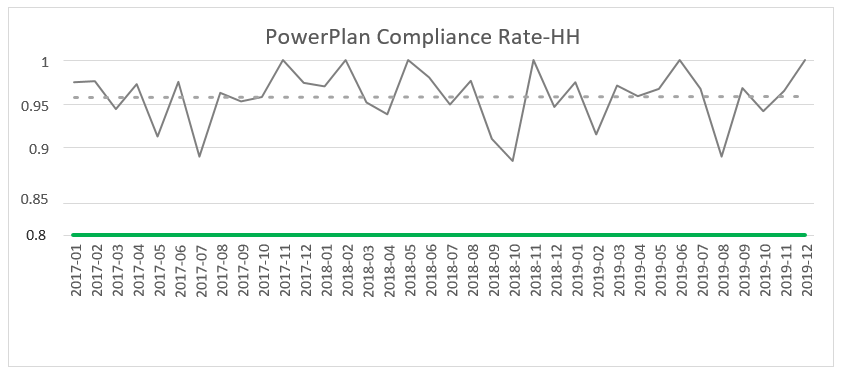
Source: Baptist Health South Florida
Improving Patient Outcomes
The overall LOS for the C-section population with the implementation of the PowerPlan decreased from 3.0 days in FY 2017 to 2.30 days in 2020 pre-COVID-19. The Premier benchmark is 2.81 days. There is a slight increase noted in LOS in Q1 2020. There also were no reported VTEs or maternal deaths within the population (Figure 11).
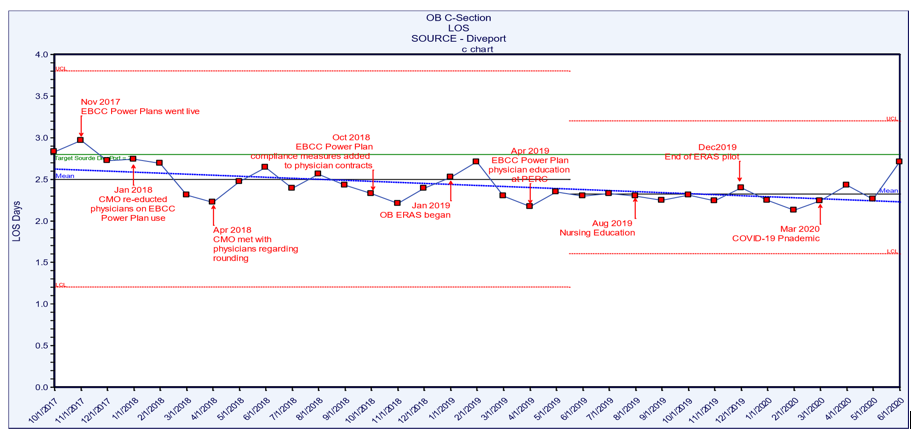
Source: Baptist Health South Florida
Of note is also the work done for the C-section ERAS pilot. This work began in January of 2019 and concluded in August of 2019 with a total of 30 patients. The outcomes for those patients included: LOS for ERAS patients as compared to non-ERAS was 1.98 vs. 2.29 for the study period. Non-Opioid use in ERAS patients was 80% and use of non-opioids in non-ERAS patients was 37.74%. The surgical infection rate for the ERAS patients was 0% and for the non-ERAS was as high as 6.25%. Pain control was also 17% better for the ERAS patients. These indicators support the evidence by showing improvements in the ERAS patients in the study. Additional utilization and process redesign will continue with ERAS projects once the impact of COVID-19 stabilizes for the organization.
Accountability and Driving Resilient Care Redesign
Creating a strong governance, incorporating evidence based clinical care and having access to a strong analytic system are all key factors in improving clinical outcomes. The data must be easily captured, readily available, meaningful to key stakeholders and the quality of the data must be trusted. BSFH has created an analytics system that is both successful and sustainable.
The EBCC is the governing body that drives the focus on reducing unnecessary cost and clinical variation through the implementation of evidence-based clinical standards integration, with real-time availability of clinical information and analytics. EBCC monitoring data is housed in DivePort 7.0 (Figure 12).
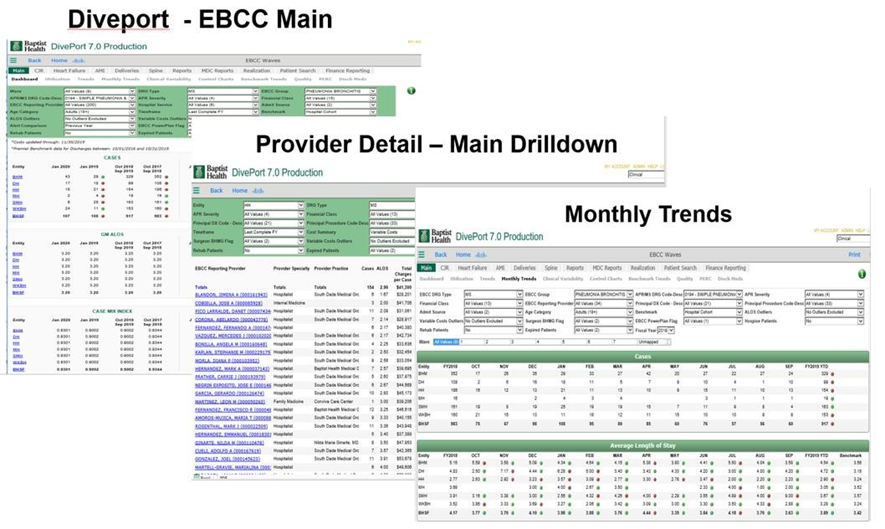
Source: Baptist Health South Florida
The implementation of the cesarean section ERAS project is a great example of how data was leveraged to trigger care and process redesign. An ERAS program consists of a multidisciplinary approach to care with a defined multimodal perioperative care pathway designed to reduce the stress response to surgery and accelerate the patient’s recovery. Successful implementation has been shown to decrease variability between patients, resulting in earlier return of gastrointestinal function and reductions in hospital length of stay, complications and total cost.
The goal of the Homestead Hospital ERAS pilot was to have 30 patients in the evaluation. This pilot study was started in January 2019 and completed August 30, 2019, with a total of 30 patients. The outcomes included a reduction in LOS, decreased utilization of opioids with an increased pain management satisfaction score and a zero surgical site infection rate, The success of the C-section ERAS pilot has led to care redesign decisions for other surgical populations. Post COVID-19 turn-around, these initiatives will be implemented on a broader scale.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



